-
Fail to pass meconium (baby's first stool/poop) in the first 24 hours
- Feed poorly
- Become distended (blown up with gas)
- Vomit
- Stool infrequently
Hirschsprung's Disease
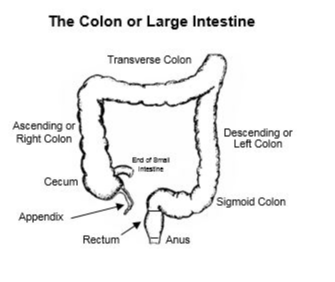
Hirschsprung’s disease is a congenital (meaning you are born with it) disease in which the end of the colon (what many people call the Large Intestine, see drawing.) behaves as it is obstructed.
The colon is a pipe which conveys stool to the anus, but it also serves as a pump. It pushes stool forward, and it does it by squeezing, and relaxing, and squeezing, and relaxing. In Hirschsprung’s disease, the system that relaxes the colon, is missing. This means that the end of the colon is always squeezing. This behaves like an obstruction and the child belly gets blown up very easily. Your child may do one or more of the following:
· Fail to pass meconium (first baby stool) in the first 24 hours
· Feed poorly
· Become distended (blown up with gas)
· Vomit
· Stool infrequently
When any of these signs or symptoms appears, your doctor may suspect Hirschsprung’s disease. If this is the case, the following are usually done:
· Abdominal x-ray – may show that the intestines are dilated up-stream from the affected segment of colon
· Contrast Enema – liquid is put in the baby’s bottom through a tube, and it fills up the colon and lights up as white on the x-ray. This can show if the end of the colon is narrower than the up-stream dilated part. That would suggest Hirschsprung’s disease, but does not make the diagnosis certain. It can help the surgeon determine how much of the colon is involved.
· Suction Rectal Biopsy – a small procedure done at the bedside to take small pieces of the rectal lining so that the pathologist can look at them under a microscope and determine if the signs of Hirschsprung’s disease are present. The pathologist looks for two major findings: The absence of Ganglion cells, and for thick nerve bundles, or what we call hypertrophic nerves. Ganglion cells are the cells that control the colon’s relaxation, and when they aren’t there, it means the child has Hirschsprung’s disease. Nerve hypertrophy usually goes along with the absence of nerve cells.
· Full-thickness rectal biopsy. Sometimes the suction biopsy is inadequate to make the diagnosis. In that case, we take a small trip to the operating room and do the biopsy directly, taking a small piece of the back rectal wall for biopsy, and closing up the hole. It is a very small procedure.
Things you should know:
1. You as a parent did nothing that gave your child this condition. Hirschsprung’s disease is relatively common, occurring in about 1 in 5000 births – sounds like a lot, but it’s not. It has been linked to some genes, but there is rarely a family history. If you have other children, you do have an increased chance of having another child with the disease. That increased risk varies depending on the sex of your child and how extensive their disease is. Your child is more likely to have a child with the disease, but those risks are still low. The disease is much more common in boys than girls, and is more common with Trisomy 21 (Down syndrome).
2. The condition is corrected with surgery. The affected segment varies in length. Most of the time the disease affects about ¼ of the colon or less. The surgery can usually be done in one stage in the newborn period. When much longer segments are affected (about 10% of the time), the surgery may be more complex. Sometimes if the diagnosis is made late, or if the segment involved is extremely long, a temporary diverting ostomy is performed before a definitive reconstruction. The choice of surgery will be made by your surgeon, explaining to you why they think a particular option is best.
3. Babies with Hirschsprung’s disease can get a condition called Enterocolitis. This is like a gastro-intestinal flu. It can be mild, or it can make them very sick, and can occur before or after surgery. It rarely occurs in older children and adults, and occurs most frequently in the first 5 years of life. It is treated with antibiotics, and rectal washouts that we call irrigations, and does the best when it is caught early. Before we make the diagnosis of Hirschsprung’s disease we usually do rectal irrigations to prevent enterocolitis, and so you should take the opportunity to become familiar with the process. We will teach you how to do them if the biopsy shows Hirschsprung’s disease, or if we are waiting for the biopsy results.
4. Constipation is the most common problem once the surgery is done. Even when you remove the colonic segment that doesn’t work well, the ‘normal’ colon is still sluggish. Nobody is sure why this occurs, but it is exceedingly common, and we expect it. We treat it aggressively and teach you how to do so, to avoid any problems in the long-term. It helps to understand that even though we can do a surgery to correct the major problem with Hirschsprung’s disease – the obstruction, you can never truly cure some of the features. This constipation is one of those features, but don’t worry. If you keep a close eye on things and prevent problems, all will be well.
5. Because the surgery does involve working near the anal sphincter, people are concerned about if their child will be continent and have normal bowel control. The answer is they should be normally continent. The overwhelming majority of patients have normal continence. Rarely a patient will have trouble with bowel control, and that may be due to surgical complication, or to long-segment disease. Even in those worst-case scenarios we offer a program called Bowel Management which ensures that a patient stays clean all the time. No matter what the situation is, we will ensure that your child’s chances are optimized for the best outcome possible, and we remain committed (for life) to ensuring that everything is the best it could be.
If you ever have any questions, we recommend you write them down and ask us. We want to make sure you understand everything so that you can be confident in the care your child is receiving.
When any of these signs or symptoms appears, your doctor may suspect Hirschsprung’s disease. If this is the case, the following are usually done:
-
Abdominal x-ray – may show that the intestines are dilated up-stream from the affected segment of colon
- Contrast Enema – liquid is put in the baby’s bottom through a tube, and it fills up the colon and lights up as white on the x-ray. This can show if the end of the colon is narrower than the up-stream dilated part. That would suggest Hirschsprung’s disease, but does not make the diagnosis certain. It can help the surgeon determine how much of the colon is involved
-
Suction Rectal Biopsy – a small procedure done at the bedside to take small pieces of the rectal lining so that the pathologist can look at them under a microscope and determine if the signs of Hirschsprung’s disease are present. The pathologist looks for two major findings: The absence of Ganglion cells, and for thick nerve bundles, or what we call hypertrophic nerves. Ganglion cells are the cells that control the colon’s relaxation, and when they aren’t there, it means the child has Hirschsprung’s disease. Nerve hypertrophy usually goes along with the absence of nerve cells. There are some other things that pathologists and surgeons look for in making the diagnosis of Hirschsprung's disease, like increased acetylcholinesterase staining, and the paucity of calretinin. Those are more advanced tests, and while they are not necessary for diagnosis Hirschsprungs disease, one or both of those tests can be useful in helping make the diagnosis. At our institution we do not do acetylcholinesterase staining, but we do stain for calretinin. I think the test is helpful, and to me it's a sign that your pathologists are staying current with what's new in Hirschsprung's disease and that your institution is probably able to handle taking care of children with Hirschsprungs.
- Full-thickness rectal biopsy. Sometimes the suction biopsy is inadequate to make the diagnosis. In that case, we plan a small trip to the operating room and do the biopsy directly, taking a small piece of the back rectal wall for biopsy, and closing up the hole. It is a very small procedure.
Hirschsprung’s disease is a significant issue, but it is easily correctible with surgery. It is not cancer, and it is not fatal. There are some risks along the way, sometimes significant, but the overwhelming majority of children with Hirschsprung’s disease do extremely well, and live full normal lives.
Hirschsprung’s disease is a congenital (meaning you are born with it) disease in which the end of the colon (what many people call the Large Intestine, see drawing.) behaves as it is obstructed.
The colon is a pipe which conveys stool to the anus, but it also serves as a pump. It pushes stool (poop) forward, and it does it by squeezing, and relaxing, and squeezing, and relaxing. In Hirschsprung’s disease, the system that relaxes the colon, is missing. This means that the end of the colon is always squeezing. This behaves like an obstruction and the child belly gets blown up very easily. Your child may do one or more of the following:
